Advance directives are important documents that outline your medical treatment preferences, but they’re only effective if they’re accessible. I can’t tell you how many times I’ve met a patient with an advance directive locked in a safe somewhere who is now too sick to tell me their wishes directly.
There are 3 steps you NEED to follow if you really want your wishes to be properly represented to the doctors down the road.
- If you’re naming someone to be your backup medical decision maker with a HCPOA document – TELL THEM. If someone is getting called in to make decisions for you, it’s usually for high-stakes stuff like whether or not to continue life support, place a feeding tube, or transition to hospice care. You HAVE to make sure your person would be willing do that sort of thing.
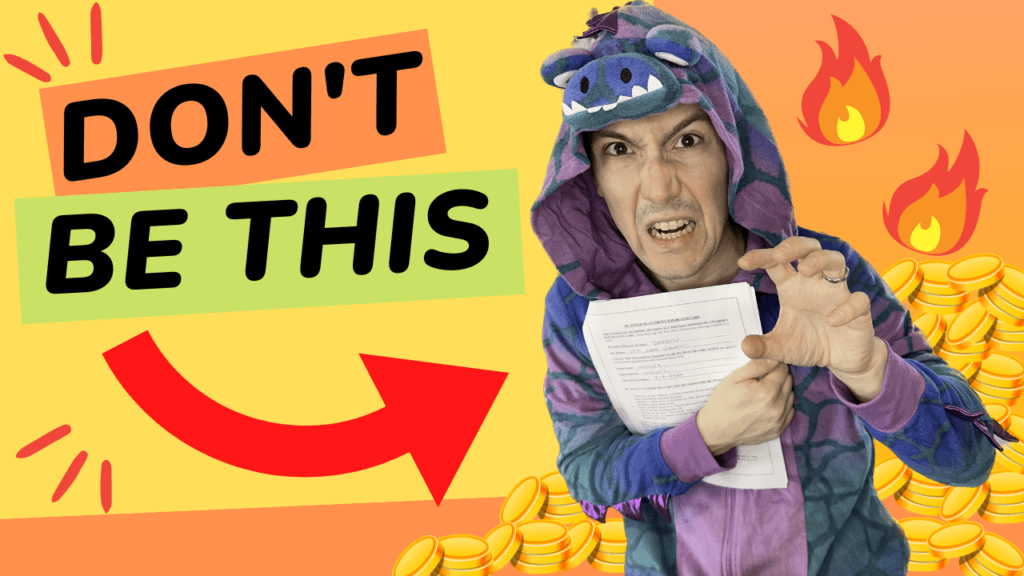
- Don’t be greedy with your advance directive! After you complete your advance directive don’t go hiding in a safe or keep the one and only copy with your lawyer. You are not a dragon and this is not your gold treasure to guard. If you get sick enough that your directive is needed, you probably won’t be physically able to get the papers yourself. Give a copy to your designated proxy decision maker for sure, but consider also giving copies of your advance directives to anyone the doctors might call in an emergency to hedge your bets.
- Walk the people who might be making decisions for you someday through your advance directives. But don’t just read the document together because most advance directives are boilerplate documents that are not that specific. You want to make sure your people understand you and your values. Make sure your proxy agent(s) understand what living means to you and what scenarios would NOT be living to you. The thing is, it’s impossible to predict the exact decisions you might have to make someday. Decisions like whether or not to accept ventilator support are hugely dependent on the context of that decision. So rather than try to predict the future, help your people understand what matters most to you, so they can prioritize that if they need to make medical decisions that include tradeoffs for you someday
Finally I want to acknowledge that if you are living with a serious illness, these conversations are harder when the hypotheticals may not be so hypothetical. At the same time, these discussions can be incredibly meaningful. So many times I’ve seen how talking about what matters most opens up deeper understanding, deeper respect and deeper love for people that have known each other for DECADES. I hope that for whatever you’re dealing with that is your experience too.
Learn more about advance directives right here: https://getpalliativecare.org/prepare…